Running and Friendly Links
Do you need an article or blog post written? I offer these services at reasonable rates. Interested? Hire Me!
Running in the Heat & Humidity
Improve Athletic Performance in the Summer Heat


This article was last revised on 08/26/17.
If there’s one thing runners in Texas understand, it’s heat. Some seem to tolerate it more than others, but too much of it can be deadly. Have you ever wondered exactly how and why it affects you like it does?
I mean the real nuts and bolts explanation? Dr. McEntire has condensed a huge body of knowledge into this concise bulleted presentation. In order to keep improving your running performance, you need to pay attention to conditions, and dial back your effort accordingly.
Read on; you’ll learn how to cope with hot weather running and perform better on race day.
- Thermoregulation1-3
- Responsible for maintaining adequate heat production and sufficient heat dissipation
- Normal skin temp: 33°C (91°F), range 32-35°C
- Normal core body temperature: 37°C (98.6°F)
- In the heat:
- Skin is only region directly vasodilated by heat stress
- Skin temperature increases before core temperature
- Skin blood flow must then increase
- Sweating begins within 2 seconds
- Exercise4-6
- Core temperature increases during exercise in relationship to exercise intensity
- Heat production is 15-20 times greater than rest
- ~70% of energy produced is released as heat instead of energy for muscles
- Causes increase in core temperature by 1°C for every 5 min of exercise w/o heat loss
- Thus heat production exceeds heat loss
- Heat & humidity:
- HR increases up to 10 bpm when temps are 75-90°F
- HR increases up to additional 10 bpm when humidity is 50-90%
- Performance decreases by ~20% when temps are above 80°F
- Heat dissipation1, 7
- What areas of body are most important for heat dissipation?
- Forehead (time to rethink that bandana?)
- Upper limbs
- Trunk
- Lower limbs
- Heat is transported by blood from muscles to skin by:
- Sweating (evaporation)
- Primary mechanism for heat dissipation
- 2/3 of evaporated fluids comes from skin (1/3 from respiration/breathing)
- 1.6-4 million sweat glands
- Sweat an average of 1.4 L/hr (max 3 L/hr)
- High humidity
- Air can’t absorb sweat so sweat drips from body
- Increased skin blood flow (convection)
- Transfer heat from core to skin
- Stimulates sweat response
- Sweating (evaporation)
- Core temperature can reach dangerous levels within 10 min w/o adequate dissipation
- Heat related illnesses
- ~240 people/year die8
- 3 types4-6
- Heat cramps-sharp stabbing pain typically in legs or diaphragm
- Caused by electrolyte deficiencies/imbalances
- Treatment-stop running, ingest a sports drink to replace fluids/electrolytes, cool body
- Exertional hyperthermia-
- Symptoms
- Core temp 39-40°C (102.2-104.0°F)
- Excess sweating causing fluid volume depletion (6-10% of body weight)
- Headache, nausea, vomiting, fatigue
- High HR
- Treatment
- Seek medical help-can progress quickly
- Fluids/electrolytes
- Cool body via immersion
- Elevate feet above level of heart
- Symptoms
- Exertional heatstroke
- Symptoms
- All of the above
- Core body temperature > 40.5° (104.9°F)
- Mental changes-confusion, disorientation, loss of consciousness
- Seizures, coma
- Organ failure
- Death
- Treatment
- IMMEDIATE medical treatment!!
- Cool body-ice/immersion
- No fluids if unconscious/severely disoriented/seizing, etc.
- Symptoms
- Heat cramps-sharp stabbing pain typically in legs or diaphragm
- Risks factors for developing a heat related illness9
- Low fitness level (<40 ml/kg/min)
- Dehydration
- Unacclimated to heat and humidity
- Overweight/Obese (BMI >27)
- Illness
- Prior heat illness
- No sleep
- Heavy clothing
- Medications/supplements
- Air temp >33°C (91°F) and/or low air velocity
- Prevention
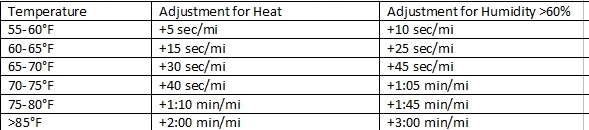
- Adjust pace for heat (~2-3 min slower per mile)
- Take walk breaks regularly & often
- Hydration
- Critical in 24 hours before a run
- Thirst is not an indicator of dehydration but increased HR and dark urine are
- Body absorbs fluids best when cold (40’F is ideal); cold fluids also help reduce core temperature
- Rule of thumb= 4-8 oz. of fluids every 15-20 min
- Calculate fluid needs/losses (nude wts best)
- Needs during run
- Wt post – Wt pre + Fluids Consumed = Total fluid lost
- Total fluid lost divided by number of miles ran = amt. of fluid needed per mile (ie 122 lb – 124 lb + 40 oz = 38 oz lost; 38 oz/5 miles = 7.6 or ~8 oz/mile to avoid dehydration)
- Rehydration
- Wt pre – Wt post = lbs lost x 16 oz (ie 124lbs – 122 lbs = 2 lbs lost; 2 x 16 oz = 32 oz needed to rehydrate)
- Do NOT drink so much water that you flush out (pee) or have too little electrolytes
- Fluids with electrolytes, eat small amts of foods w/sodium 12 hrs before
- Hyponatremia-abnormally low sodium levels, excess water moves into cells, causing them to swell/burst
- Symptoms can mimic heat illness
- Elevated core temperature
- Nausea/vomiting
- Headache, confusion, irritability
- Fatigue
- Muscle weakness
- Seizures
- Loss of consciousness, coma10
- Symptoms can mimic heat illness
- Acclimation7, 11, 12
- ~2 weeks of moderate intensity exercise, 30-100 min in duration in the heat
- Kids need ~ 2x the number of sessions
- Adaptations can be lost in as little as 10 days
- Results in:
- More sweat production but less sodium lost in sweat
- Better control of core body temperature fluctuations
- More efficient heat dissipations mechanisms
- Time of day
- Early morning or evenings
- A good rule of thumb is to run when your shadow is taller than you are!
- Avoid running between 12-3pm
- Clothing
- Light-colored, breathable, moisture-wicking fabric
- Sunscreen
- 8 oz. cotton t-shirt can soak up 4x its wt. in sweat making it weigh 2 lbs-yikes!
- Switch from a hat to a visor
The bottom line is not to approach hot weather running full-out if you are not prepared for it. And make sure that you warm up properly. If you live and train in an area that gets very hot in the summer acclimation will be a natural progression as you transition from spring to summer.
However, if you live in a cooler area and travel to a hotter destination for vacation or work, approach your running there carefully. Do you have any tips on this topic? Scroll down and share them with other readers!
About the author: Serina McEntire, PhD, is an Exercise Physiologist in the Dept of Emergency Medicine at the University of Pittsburgh. She has more than 10 years experience in the health and fitness industry working with a wide range of clients. She also coaches a half marathon training group.
Visit Kelly's profile on Pinterest.
References:
- Rowell, L.B., Human Circulation: Regulation During Physical Stress. 1986, New York, NY: Oxford University Press. p. 174-212.
- Johnson, J.M. and D.W. Proppe, Cardiovascular adjustments to heat stress., in Handbook of Physiology. Environmental Physiology. 1996, Am. Physiol. Soc.: Bethesda, MD. p. 215-243.
- Rowell, L.B., Cardiovascular adjustments to thermal stress., in Handbook of Physiology. The Cardiovascular System. Peripheral Circulation and Organ Blood Flow., J.T. Shepherd and F.M. Abboud, Editors. 1983, American Physiological Society: Bethesda, MD. p. 967-1023.
- Barrow, M.W. and K.A. Clark, Heat-related Illnesses. American Family Physician, 1998. 58(3): p. 749-756, 759.
- Armstrong, L.E., D.J. Casa, M. Millard-Stafford, D.S. Moran, S.W. Pyne, and W.O. Roberts, American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc, 2007. 39(3): p. 556-572.
- Armstrong, L.E., Y. Epstein, J.E. Greenleaf, E.M. Haymes, R.W. Hubbard, W.O. Roberts, and P.D. Thompson, American College of Sports Medicine position stand. Heat and cold illnesses during distance running. Med Sci Sports Exerc, 1996. 28(12): p. i-x.
- Shibasaki, M., T.E. Wilson, and C.G. Crandall, Neural control and mechanisms of eccrine sweating during heat stress and exercise. J Appl Physiol, 2006. 100(5): p. 1692-1701.
- CDC. Heat-related illness and deaths-United States, 1994-1995. MMWR Morb Mortal Wkly Rep., 1995. 44: p. 465-468.
- Armstrong, L.E., D.J. Casa, M. Millard-Stafford, D.S. Moran, S.W. Pyne, and W.O. Roberts, American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc, 2007. 39(3): p. 556-572.
- http://www.bing.com/health/article/mayo-126647/Hyponatremia?q=hyponatremia
- Armstrong, L.E. and C.M. Maresh, Exercise-heat tolerance of children and adolescents. Pediatr Exerc Sci, 1995. 7: p. 239-252.
- Johnson, J.M., Physical training and the control of skin blood flow. Med Sci Sports Exerc, 1998. 30(3): p. 382-386.
Recommended Related Articles
- The Columbia Omni Freeze Zero Shirt
- Stress Fracture or Shin Splints?
- Is Your Mineral Intake Adequate?
- Specific Stretches Relief for Runner’s Knee
- All Natural Exercise Supplements that Work
Website © 2010 KSmith Media, LLC; all rights reserved; content may not be copied, rewritten, or republished without written permission. Webmaster’s Google profile